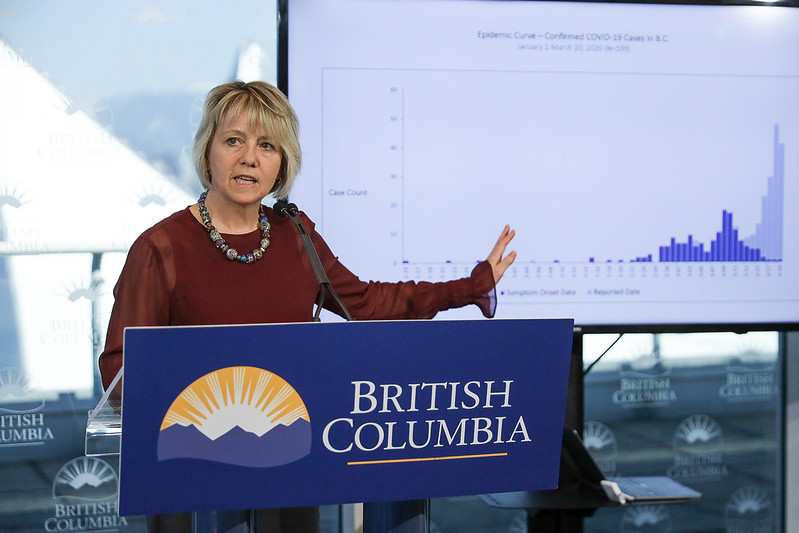
To provide clarity on strategies being used by public health authorities, Dr. Bonnie Henry, Provincial Health Officer, offered an explanation into B.C.’s COVID-19 testing strategy.
“Many have asked and many continue to ask about who is getting tested for COVID-19 in B.C. and why we don’t just ‘test, test, test everyone.’ What I can tell you is we adapted our testing approach as we learned more about the virus and the test, and as more tests became available, and we will continue to adapt as we progress through our pandemic response,” said Henry.
Henry said that scientists working in the BCCDC were among the first in the world to develop a test.
“This test detects the genetic material of the virus in a sample (usually a swab taken from the back of the nose) from someone who is sick. It is used across Canada and around the world to determine if someone is infected.”
At the start of the pandemic, the testing strategy focused on the source of transmission to understand who was getting and spreading the illness to better guide the province’s response.
“That’s why we first focused on returning travellers, in combination with leveraging our annual active influenza surveillance testing. This allowed us to put in place the necessary precautions, orders and restrictions we have today,” explained Dr. Henry. “As the pandemic progressed in B.C. and we had evidence of community transmission, we adapted our testing strategy to focus on those most vulnerable to serious illness from COVID-19.”
The strategy shifted, according to Henry, because officials knew the virus was potentially everywhere, and many people with mild symptoms could self-isolate at home.
“We concentrated on the sickest patients, health-care workers, those in long-term care homes and those connected to an outbreak. This gave us an understanding of the impact of COVID-19 on hospitals and care homes.”
Testing was only part of the strategy to contain the virus as best as possible, as contact tracing is and will continue to be important as the province moves into Phase 2 of BC’s Restart Plan.
When new case rates began to slow around mid-April, Dr. Henry said that the strategy shifted once again, to allow anyone with symptoms of COVID-19 to get tested, however, there are still some flaws to be worked out.
“It’s still important to remember not everybody needs a test and the tests we have are not perfect. If someone tests negative, it may mean they are too early in the illness for the test to detect it yet – a false negative,” said Henry. “When we have a small number of people who actually have COVID-19 in the population, the number of false positives can also be very high. That means we are telling people they are infected and may be immune to COVID-19 when they aren’t.”
Henry added that the next step that health officials plan to make will be the introduction of a serology test, which can detect COVID-19 antibodies in people who have become infected in the past.
“Once the serology test has been validated for accuracy, the test results will be used to get a better sense of where the virus has been and how to further prevent its spread as we move into the next phase of our pandemic.”
Henry added that the strategy was never a blanket test of every B.C. resident, as the tests have their limitations, but rather to use it strategically to best protect British Columbians. However, Henry believes that the strategies employed in B.C. have been effective so far.
“Our strategy is working, even as we develop it further to meet our evolving needs. It is adapted to our pandemic experience that is helping all of us to hold the line and get through this storm. It will continue to support us as we move through the next phases of this challenging pandemic,” concluded Henry.